Talk Test Treat Trace
Chapter 3: Increasing the uptake of testing
In this chapter
Key points
- Early detection and treatment of sexually transmitted infections (STIs) and blood-borne viruses (BBVs) aims to:
- interrupt ongoing transmission
- prevent or limit adverse outcomes
- reduce the risk of human immunodeficiency virus (HIV) transmission
- reduce the prevalence of STIs and BBVs in the community.
- Ensure testing is directed to 15 to 30 year old people and other priority populations at regular time intervals and avoid asymptomatic screening of low prevalence populations.
- Integrate testing of 15 to 30 year old people into routine health screening, reproductive health checks and opportunistically at other visits.
- Provide appropriate information on STIs and BBVs to enable prevention, harm reduction and encourage health-seeking behaviour that leads to the uptake of testing.
- Ensure that health services and staff provide an environment that is accessible and acceptable for priority populations.
- Understand when a comprehensive sexual history and check-up should be conducted and when it is not necessary and can be simplified.
- Simplify obtaining consent to testing to make it quick, easy and acceptable to clients and practitioners.
- Ensure that health information system (HIS) templates and recalls align with recommendations for STI and BBV testing.
Epidemiology
STIs and BBVs can affect anyone of any age, either because of their own or their partner’s behaviour, or because they are in a certain age or risk group among whom infections are common. The pattern of distribution of STIs and BBVs among populations and regions is well defined, and regardless of individual risks, the majority of treatable STIs occur among 15 to 29 year olds. With regard to chlamydia, 73 per cent of all notifications occur among 15 to 29 year olds, with 15 to 19 year old women being the highest risk age group. Among 15 to 24 year olds, national surveillance reports indicate chlamydia is detected in about 1 in 20 tested (5.9 per cent) through primary health services. Between 2008 and 2013, 36 clinical audits of STI testing and treatment were conducted at 16 Aboriginal Community Controlled Health Services (ACCHS) in both urban and remote areas of Western Australia (WA), New South Wales (NSW), Northern Territory (NT) and Queensland (Qld). These audits identified very high chlamydia positivity rates that were consistent across services, regardless of location. Among all women tested for any reason, chlamydia was detected among 10 per cent of all antenates, about 20 per cent of all 15 to 24 year olds and 25 per cent of 15 to 19 year olds. About 50 per cent of these women were tested as part of routine asymptomatic screening.
In contrast to chlamydia, the rates of gonorrhoea, trichomonas and syphilis vary with geographic location and increase with remoteness, which is also associated with less availability of and access to clinical services. Before the introduction of the diagnostic tool polymerase chain reaction (PCR), the inability to detect some infections due to limited access to laboratories, has also contributed to the higher rates of gonorrhoea, trichomonas and syphilis in remote areas. Consequently, young people living in remote areas are at much higher risk of several STIs compared to those living in urban areas, simply because they are sexually active within a community where those infections are very common and easily transmitted.
Early detection and treatment
STIs are frequently asymptomatic or cause minimal signs and symptoms that can go unrecognised both by those affected and practitioners. Because of the asymptomatic nature of many infections, early detection and treatment of people known to be at risk is a core component of our STI and BBV strategies. Early detection and treatment aims to:
- interrupt ongoing transmission
- prevent or limit adverse outcomes such as:
- adverse reproductive health outcomes (e.g. pelvic inflammatory disease [PID], chronic pelvic pain, infertility)
- adverse outcomes in pregnancy (e.g. ectopic pregnancy, miscarriage, premature rupture of membranes, post-partum and neonatal infections)
- cirrhosis and liver cancer
- progression to severe immune suppression and acquired immunodeficiency syndrome (AIDS)
- reduce the risk of HIV transmission
- educe the prevalence of STIs and BBVs in the community.
There are many circumstances when individuals with symptoms or specific risk factors should be tested for STIs and BBVs. Nevertheless, to be cost-effective at a population level, early detection and treatment should be directed to those who are known to be at high risk of STIs. With regard to testing and treatment, it is also important to take into account what infections are common, and therefore likely in the region or among specific priority populations.
Reducing barriers and increasing the uptake of testing among priority populations
Barriers to testing for STIs and BBVs are varied and may include:
- client factors: fear, shame, embarrassment, lack of knowledge or awareness, gender of practitioner or relationship of practitioner to the client
- practitioner barriers: personal barriers with regard to talking with clients about sex, fear of not being the appropriate gender to the client, lack of knowledge or confidence, lack of time or competing priorities
- the way in which it is offered: real or perceived lack of privacy and confidentiality or the way in which the subject is approached or questions asked
- health services and systems: STIs and BBVs may not be prioritised or well supported at a health service level, systems may not support easy testing and treatment, continuous quality improvement (CQI) may not be carried out or used effectively to identify and address barriers.
Although some of these barriers may be difficult to address, others can be reduced in a way that enhances the uptake of STI and BBV testing among priority populations. These include:
- providing an appropriate service that is confidential, non-judgemental, non-discriminatory, and is accessible and acceptable to the priority population
- providing appropriate information on STIs and BBVs to enable prevention, reduce harm, and encourage health-seeking behaviour that leads to proactive access to early detection and treatment
- ensuring testing is directed to those at highest risk at appropriate time intervals (avoid testing low prevalence populations)
- integrating testing into routine primary healthcare delivery
- simplifying obtaining consent to testing to make it straightforward and easy
- ensuring that testing is offered in an appropriate way that leads to an increase in the uptake of testing
- understanding when a comprehensive sexual history and check-up should be conducted and when it is not needed, or understanding when it can be simplified to make it quick, easy and more acceptable to clients and practitioners
- using CQI to identify and address barriers to testing.
Providing appropriate service and information
Providing appropriate information and education on STIs and BBVs to the community in general and specifically to those at highest risk enables people to make informed choices to reduce their individual risk such as through prevention and harm reduction strategies. Providing education and encouraging health-seeking behaviour empowers people to be proactive in their healthcare, including accessing services to request testing for STIs and BBVs. At the same time, health services must also provide an environment that is acceptable and enables access for clients. Displaying health promotion materials that promote and normalise testing for STIs and BBVs can assist practitioners to offer – and clients to request – STI and BBV testing. More detail about enabling environments and education are provided in Chapters 1 and 2.
Ensure testing is directed to priority populations at regular intervals
In addition to ensuring STI and BBV testing is primarily directed to all 15 to 30 year olds, be familiar with other priority populations in the community, what tests should be taken and how often. Understand the difference between testing someone of any age when they present with signs or symptoms or specific risk factors, as well as what tests should be taken in the context of routine asymptomatic testing. Remember that concurrent infections are common and that being at risk of one STI or BBV indicates risk for others. Offer testing for all STIs and BBVs (chlamydia/ gonorrhoea/trichomonas* , syphilis, hepatitis Bϯ and C, HIV) when people present for any of the following reasons:
- STI or BBV has been detected on asymptomatic screening
- they present with signs or symptoms that could be due to an STI or BBV
- their own or their partner's history indicates specific risk factors
- they have had a recent change in sexual partner
- they are a contact of someone with an STI or BBV
- they are pregnant where the consequences of not detecting and treating STIs and BBVs have potentially serious adverse outcomes
- they request a sexual health check-up
* Add trichomonas PCR if at risk or living in an endemic area
ϯ Add hepatitis B if never tested before or hepatitis B status is unknown
How frequently should asymptomatic testing be offered?
As with other health screening, testing for STIs and BBVs should occur routinely at regular intervals among people who are at risk but who have no symptoms (asymptomatic testing) to enable early detection and management. Table 1 outlines the recommendations for testing among certain priority populations. Be mindful that an individual client's risk may make it appropriate to test for more STIs and BBVs and more frequently than the minimum outlined in the table. Table 1 is a summary of WA and national protocols and provides a guide to testing, particularly in the context of the syphilis outbreak and high rates of STIs. More information on STI and BBV testing and what specimens to collect can be found in the Silver Book and the Australian STI Management Guidelines:
http://ww2.health.wa.gov.au/Silver-book
http://www.sti.guidelines.org.au/
Table 1. Recommended frequency of asymptomatic testing
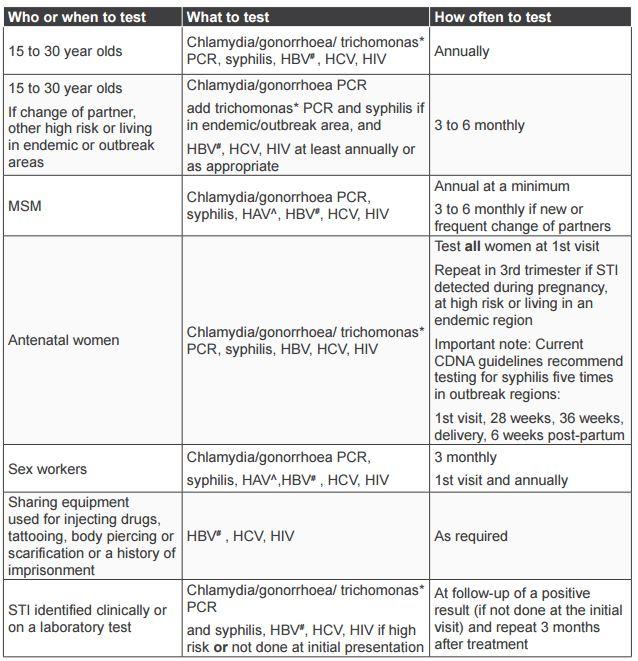
HAV = hepatitis A virus; HBV = hepatitis B virus; HCV = hepatitis C virus
* If at risk or living in an endemic area including the Pilbara, Goldfields, Midwest and Kimberley regions
# HBV test at first visit or if immune status is unknown. No need to test if immune or immunisation completed. Offer immunisation if not immune
^ HAV test at first visit or immune status unknown for MSM and sex workers. No need to repeat if immune or immunisation completed
The pattern and distribution of infections can change over time, such as when new infections emerge or outbreaks occur. Be familiar with local epidemiology and current recommendations regarding STIs and BBVs among age and risk groups as well as identifying changes and directing strategies in response.
Who should not be offered routine asymptomatic screening at a population level?
While STIs and BBVs can affect anyone of any age, most infections occur among 15 to 30 year olds and relatively few occur among people aged over 40 years. Asymptomatic screening of low risk populations, such as those aged over 40 years, not only results in very low detection of cases but diverts significant time and resources away from where they should be focused. It is therefore not cost-effective and not recommended.
Effective case detection and management among low-prevalence populations relies not on asymptomatic screening but on ensuring appropriate testing of individuals who present with a specific risk history, with signs and symptoms, as a contact of someone with STIs and BBVs or who request testing. HIS templates and recalls, such as the adult health check, should be consistent with the recommendations for asymptomatic screening of STIs and BBVs with regard to age groups and frequency of asymptomatic screening.
In all regions, asymptomatic screening of chlamydia and gonorrhoea should be directed to 15 to 30 year olds. Extending the upper age limit to 35 or 40 years should be guided by local epidemiology.
Note that the epidemiology of trichomonas is different from that of chlamydia and gonorrhoea with regard to the age range affected. In areas where trichomonas is endemic, prevalence is highest among 15 to 30 year olds but is not confined to that age group and extends into older age groups. Untreated, women can remain infected with trichomonas for years; therefore, detection among older women is not necessarily a sign of recent acquisition. Case detection and treatment of trichomonas among older women relies on a combination of ensuring appropriate PCR testing when women present with signs and symptoms or a risk history as well as detection on routine cervical screening.
*Note that with regard to pathology request forms, it is preferable to request testing due to the presence of symptoms or 'STI risk' rather than to request an 'STI screen'.
Integrating early detection and treatment into routine primary healthcare
Early detection and treatment is an important strategy that includes testing people who are at risk but who are asymptomatic, as well as those who have signs and symptoms. STIs and BBVs can be truly asymptomatic or cause minimal signs and symptoms that go unrecognised by both those affected and health practitioners. The ability to recognise and present with those signs and symptoms is impacted by many factors including the knowledge and experience of both clients and practitioners as well as health-seeking behaviour. The development of symptoms from the time of infection with STIs and BBVs is variable, but can take months to years, providing a long timeframe for potential transmission to others. Early detection and treatment is therefore an important strategy to detect infections early and prevent or limit the development of complications and interrupt ongoing transmission.
The principles of early detection for STIs and BBVs are no different from many other health issues that are routinely screened for through primary health services. Primary health services often use a variety of ways to conduct testing for STIs and BBVs. Where appropriate, STI and BBV screening should be integrated and conducted at the same time as other health screening activities, such as antenatal screening and adult health checks. Screening may also be conducted in the context of outreach programs, which are discussed in more detail in Chapter 5. STI and BBV testing should be an integral part of routine health screening in the following circumstances: antenatal screening adult health check for 15 to 30 year olds cervical screening up to 30 years.*
*Extending the upper age limit to 35 or 40 years should be guided by local epidemiology.
Integrating early detection into routine visits for young women
Young women present frequently to primary health services for reproductive health issues, providing many opportunities to integrate STI testing in a simple and straightforward way. A urine sample is often taken as part of those consultations, making sample collection for PCR easy.
Common presentations among young women who are, or plan to be, sexually active include:
- pregnancy tests (positive and negative results)
- pre-pregnancy check-ups
- contraception
- urinary tract infection (UTI)
- referral for termination of pregnancy (TOP)
- insertion of an intra-uterine device (IUD)
- other reproductive health issues.
Ideally, when testing for STIs at the same time as conducting a pregnancy test, regardless of whether a woman wishes to proceed with the pregnancy or not, women should be tested for chlamydia, gonorrhoea and bacterial vaginosis (BV). The early detection and management of these infections can prevent early miscarriage and the development of PID following miscarriage and TOP.
Integrating testing into routine visits for young men
While young women bear the burden of ill health from STIs, the failure to engage young men in early detection and treatment programs contributes to high rates of reinfection of women and ongoing transmission in the community. The current large disparity and low rates of testing among young men compared to young women is not simply explained by men not presenting to primary healthcare services or by the absence of male practitioners. While a lack of male practitioners is an issue for many services, very low rates of testing among young men have been reported from many health services with an adequate number and range of male health practitioners.
Young men do present to primary health services but in fewer numbers than young women and significantly much less frequently and rarely for reproductive health visits, resulting in fewer opportunities to offer testing. This highlights the need to ensure testing is maximised by integrating testing into all visits where possible and appropriate. In particular, testing of 15 to 30 year old males should be integrated routinely into health screening, such as adult health checks, and offered opportunistically at other visits in a way that is easy, simple and likely to lead to the uptake of testing.
Integrating tests into outreach programs
Conducting STI and BBV testing in the context of outreach programs can be an effective way to reach people at risk who may be marginalised or who have difficulty accessing health services. Outreach programs can consume a lot of time and resources; they should be well targeted and evaluated. Do not try them before ensuring that testing is well integrated into existing primary healthcare services that are, or could be, accessed by specific age and risk groups. While Chapter 5 provides more detail about conducting outreach programs, note that the principles of testing as discussed in this chapter should be consistent regardless of the context.
How to increase the uptake of testing
The principles of asymptomatic screening for STIs and BBVs are no different than testing for any other health issue with regard to consent, confidentiality, who testing is offered to and how frequently, and the follow-up of abnormal test results. Currently, STI and BBV screening is well integrated into routine antenatal screening but the integration into other routine health screening, such as adult health checks, is variable with low STI screening rates among women in the highest risk age group (15 to 19 years) and young men in general.
To address barriers to STI and BBV testing among those at highest risk, it is important to acknowledge that barriers exist and to identify the ones that can be mitigated. Antenatal screening can be used as a model or guide to how STI and BBV screening has been integrated into routine screening in a way that is universally offered, easy, simple and acceptable to both clients and practitioners.
*Extending the upper age limit to 35 or 40 years should be guided by local epidemiology.
Some of the factors that directly impact the ability of practitioners to offer testing and for clients to agree to the uptake of testing include:
- gender or the relationship of the practitioner to the client
- experience, expertise and confidence of practitioners
- whether a sexual history is taken or not
- whether testing is offered using an opt-off versus an opt-on approach
- how consent is gained
- whether testing has been integrated into routine primary healthcare delivery
- whether HIS support and facilitate routine testing.
Gender or the relationship of the practitioner to the client
Practitioners may be concerned that their gender or relationship to the client may make it difficult or inappropriate to gain consent to testing for STIs and BBVs. Be mindful that while these factors might be an issue for some people, they might not be for others. Remember that all clients have a right to have access to the best available health care and to be provided with information to enable them to make informed decisions.
In ideal circumstances where many options are available, individuals may choose to see a particular practitioner for a variety of reasons. However, in many settings those options are not readily available and often people will make a choice to access a health service despite the lack of a practitioner most appropriate or acceptable to them. Be careful not to make assumptions about what is or isn’t acceptable to individual clients.
Rather than avoiding the subject or denying someone access to testing and management, the easiest way to assess whether you are the appropriate practitioner for them is to simply ask permission in a sensitive, respectful but straightforward manner. This may involve asking upfront if they are happy to see you or whether they would prefer to see another practitioner, or asking during the consultation whether it is OK if you ask them some specific questions to assess whether they might be at risk of an STI or BBV, or to conduct an examination.
Experience, expertise and confidence of practitioners
While experience and expertise make taking a sexual history, conducting an examination and providing appropriate management easier, a lack of expertise should not create a barrier or an excuse for not conducting tests for STIs and BBVs. While not all practitioners are experts in antenatal care or diabetes management, all practitioners working in primary healthcare services should be able to provide a minimum of information to clients to gain consent to testing and to take specimens required in the context of screening. If an abnormal result is identified or symptoms are apparent, clients can be referred to a more appropriate or experienced practitioner to provide more information or management. In the same way, practitioners do not need to have expertise in STI or BBV management in order to gain consent and obtain specimens for testing. If issues arise during the course of conducting screening or an STI or BBV is detected on screening, clients can be referred as appropriate. But testing should not be deferred due to the risk of loss to follow-up.
Does a sexual history need to be taken?
Taking a detailed sexual history before asymptomatic screening for STIs and BBVs is ideal but not always practical or necessary. With regard to routine testing, being aged 15 to 30 years alone determines that testing should be offered. While taking a history or risk assessment can be valuable, it is not necessary to determine whether testing should be offered to this age group and can create barriers to testing for both practitioners and clients.
Other factors that can also make it difficult or impractical to take a sexual history include that practitioners may lack confidence, may have limited time and may have competing priorities. Clients might find it confronting to be asked about their sexual history, especially if they are young or have presented for unrelated reasons.
STI and BBV testing also often occurs in the context of more comprehensive check-ups, such as adult health checks or antenatal screening or opportunistically when they present for other reasons. In those circumstances, even though it might not be practical or appropriate to ask for a detailed sexual history, you should not be deterred from offering testing in a simple and easy way. It is far preferable to encourage the uptake of testing among those at high risk and to take a history at follow-up if an STI or BBV is detected than not to offer testing because of the inability to take a thorough history at that time.
If a sexual history and risk assessment is warranted, it can also be simplified by asking a few key questions in an appropriate manner. At a minimum, a few simple questions such as those shown below can provide useful information and may lead to more detailed questions being asked.
- Do you have a regular partner? If so, how long have you been together? When was the last time you had sex with your regular partner?
- When was the last time you had sex with a different partner?
- When was the last time you used a condom for sex? Do you use condoms with your regular and/or casual partners?
- Ask some specific questions about STI symptoms: have you noticed any low abdominal pain, abnormal bleeding (women), pain on passing urine, discharge or genital sores or rashes (both).
The reason for presentation, the context of testing, the expertise of the practitioner and the time available will all contribute to whether a sexual history or risk assessment is practical or if it is needed at all in order to determine whether testing should be offered and gaining consent to testing.
Remember that a detailed sexual history and risk assessment should always be taken if possible, or at least simplified, when someone:
- presents with signs or symptoms that could be due to a STI or BBV
- presents as a contact of someone with a STI or BBV
- presents at follow-up if an STI or BBV was detected on an asymptomatic screening test
- requests a check-up.
More information about taking a detailed sexual history and examination can be found in the Australian STI Management Guidelines and the Silver Book available via the links below:
http://www.sti.guidelines.org.au/
Gaining consent to testing
Regardless of the context of testing, clients should always be informed about what they are being tested for and why it is important. They should also provide verbal consent to testing. Always ensure the client’s privacy and confidentiality and use a sensitive and respectful approach. Gaining consent does not need to involve a lengthy discussion but should provide a brief explanation of what is being tested for and why, and provide an opportunity for clients to ask questions. Make sure you explain what will happen if any result needs to be followed up, clarify how they would like to be contacted and check that contact details are up-to-date. With regard to notifiable diseases, clients should be informed that the Department of Health receives confidential positive test results. All the named results are stored on the confidential database called the WA Notifiable Infectious Diseases Database (WANIDD). Access to this database is restricted to epidemiology and surveillance staff working at the Communicable Disease Control Directorate (CDCD) at the Department of Health and disease control doctors and nurses at regional Public Health Units (PHUs).
Clients should also be informed about My Health Record. The specific information that needs to be discussed will vary depending on their age, whether it has already been discussed and clarified at a previous consultation, and whether clients have already chosen to opt-on or opt-off. More information about My Health Record with regard to STI and BBV testing can be found on the Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine (ASHM) website and the Australian Government Digital Health Agency website.
A Guide to My Health Record: for BBV and STI healthcare providers to support their patients has been developed by ASHM is available via the links below:
Australian Digital Health Agency, Australian Government. How to Take Control of Your Record From Age 14.
https://www.myhealthrecord.gov.au/for-you-your-family/howtos/take-control-your-record-age-14
Opt-off versus opt-on approach to testing
Be mindful that the way in which testing is offered and questions are asked can have a significant impact on whether someone will consent to testing or not. Using an opt-off approach, as used with antenatal screening, rather than an opt-on approach is much more likely to result in the uptake of testing. An opt-off approach refers to the practitioner informing clients who have already been identified on their basis of their age or other factors that routine testing is offered to them at regular intervals, why and what it involves. Clients have the right to decline but are less likely to if they understand that these tests are offered routinely, why they are being offered, and that testing is quick and easy.
In contrast, an opt-on approach is when the client is asked if they think they are at risk of STIs or need a check-up with questions such as, “Do you think you might have an STI? Do you want to have an STI check-up?” Questions asked in that way without an explanation that testing is offered to all young people (and why and how easy it is) can be confronting. They are likely to be answered in the negative and are much less likely to lead to an acceptance of testing. While some people might be well informed about their risks for STIs and BBVs, the asymptomatic nature of infections, what tests are involved and how often they should be tested, many other people, particularly adolescents, may not be aware of those issues and may not know that they are at risk. Remember, it is not up to clients to necessarily have a good understanding of specific STIs and BBVs and what test are required for each, so always make sure you clarify exactly what STIs and BBVs are tested for by different specimens.
In a similar way, asking a young person whether they are sexually active can be confronting, is often misunderstood and may put people offside or make them fearful of why you are asking. While young women aged 15 to 19 years are the highest age risk group for STIs, many in that age group are not yet sexually active. Rather than asking them if they are, it is much easier to use an opt-off approach to determine whether they are sexually active. When you inform them that a check-up for STIs is being offered to all 15 to 30 year olds, if they have never been sexually active they are likely tell you that and that they don’t need to have that test. Approaching the subject in this way can also enable further discussion about whether they want to ask any questions about STIs or contraception. In contrast, asking whether they are sexually active at the start is unlikely to enable a conversation about sexual health.
Table 2. Integrating STI and BBV testing into routine antenatal and adult health check screening: enhancers and barriers to the uptake of testing.
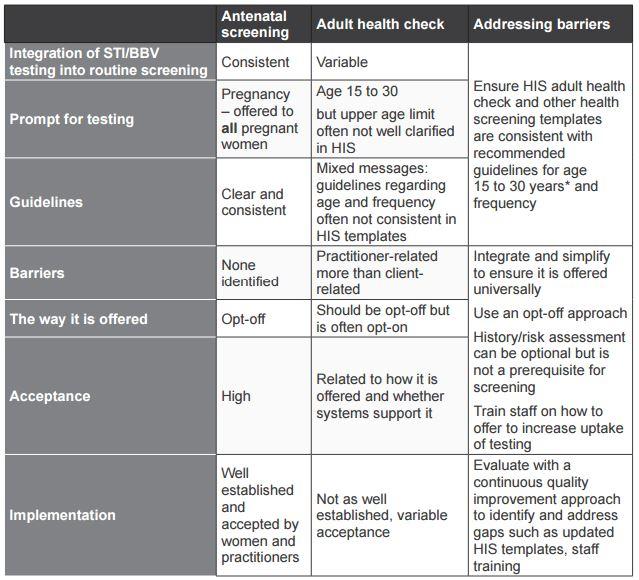
* Extending the upper age limit to 35 or 40 years should be guided by local epidemiology
HIS templates, prompts and recalls
Ensure that the templates, prompts and recalls used for routine health screening such as adult health checks, antenatal and cervical screening are consistent with the recommendations with regard to age and frequency for screening. Review and update templates for routine STI and BBV screening and recalls to ensure that:
- age parameters and frequency for testing are consistent with guidelines, in particular:
- annual STI testing for all 15 to 30 year olds
- six-monthly testing for 15 to 30 year olds, if at higher risk or living in an endemic area
- clinical or laboratory diagnosis of chlamydia or gonorrhoea prompts a three-month recall for retesting to check for reinfection
- prompts for PCR testing are embedded as a minimum and for BBVs as an option
- prompts for taking a sexual history or risk assessment are optional and not a prerequisite for testing.
Many templates currently in use for adult health checks have a tick box to identify that a discussion regarding sexual history or risk assessment has been conducted rather than explicitly prompting for STI and BBV testing. While discussion or history taking is always preferable, it is not a prerequisite for routine screening or an indicator that screening has been conducted, and it can create barriers. It can be in templates as an option but should not be a mandatory requirement for conducting STI and BBV screening among identified age and risk groups. A tick box should be included to indicate that a PCR for chlamydia and gonorrhoea has been done at a minimum and blood for BBVs as an option.